Central Oregon's Chief Pediatric Counseling Clinic

How the Brain Responds to Trauma
Derick E. Vergne, MD.
September 24, 2014
Medscape Multispecialty.
 Extreme terror is an advantageous evolutionary emotion designed for protection against real danger by prompting the person experiencing it either to fight or to flee. This classic “fight or flight” response is basically one and the same, with self-preservation as the common denominator.
Extreme terror is an advantageous evolutionary emotion designed for protection against real danger by prompting the person experiencing it either to fight or to flee. This classic “fight or flight” response is basically one and the same, with self-preservation as the common denominator.
Once the potential danger disappears, the experience of fear and terror is no longer needed, yet it may persist. In fact, continuous fear (when no longer needed to survive) becomes disadvantageous to the organism, because these feelings will prevent it from effectively looking for food and shelter, thereby threatening its very survival.
The abnormal psychological and physical experience of fear in safe or neutral situations long after the initial traumatic experience has passed is diagnosed as post-traumatic stress disorder (PTSD), or anxiety disorder. Variants in the quality and timing of the experience of danger lead to diverging diagnoses as generalized anxiety and phobias. The question is, how is experience turned into physiology—or more accurately, what are the neurobiological underpinnings of fear, and how are those activated by experience?
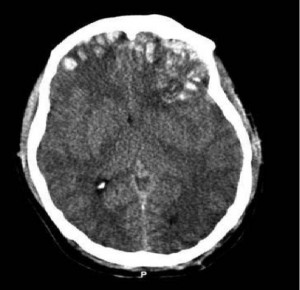
The amygdala is a well-known epicenter for the emotional “understanding” of stimuli. In other words, the amygdala helps the brain to remember the averseness of otherwise neutral stimuli.[1] Therefore, the amygdala is an integral part of the circuitry maintaining memories for aversive events.
An increasing amount of research in recent years has been geared toward defining circuitry and neurotransmitter abnormalities in patients with anxiety disorders, be it generalized anxiety or PTSD.[2] Clinical studies based on animal data consistently point to amygdala hyperactivity in anxiety disorders.[3]
To better grasp the extent to which the amygdala relates to fear and the stress response, it is much easier to think about the fight-or-flight mechanism. For instance, when the zebra notices the staring lion—or the human notices the approaching deadline, accompanied by a frowning, angry boss—the amygdala is immediately activated, followed by hypothalamus stimulation of the pituitary, ultimately causing the adrenal glands to secrete cortisol (the classic stress hormone).[4] Cortisol induces release of the stress neurotransmitters norepinephrine and adrenaline, with the accompanying sympathetic (elevated heart rate, tremors, pounding heart, and slow digestion) and psychological (fear, apprehension) changes.
Although further discussion is beyond the scope of this article, the extrahypothalamic stress axis is another way in which brain uses norepinephrine through the amygdala, bypassing pituitary and adrenal cortisol. The extra-hypothalamic stress axis is purported to be important in the perpetuation of the stress response and its psychological sequela, anxiety.[5] The amygdala is therefore a key component of the stress response.
What differentiates the generally calm individual from the chronically anxious person is not necessarily that one has “high” vs “low” amygdala function, but specifically the way in which the amygdala communicates with the “thinking part” of the brain. How does the brain think it through to modulate its activity? Research is now concentrated on clarifying how the prefrontal cortex (thinking brain) and the amygdala (primitive fear structure) communicate to modulate anxious states. Clinical neuroimaging studies have begun to clarify the neuroanatomical and neurochemical relationship between the prefrontal cortex and amygdala in the regulation of the stress response and anxious states.
References
Davis M. The role of the amygdala in fear and anxiety. Annu Rev Neurosci. 1992;15:353-375. Abstract
Charney DS, Nestler EJ, Sklar P, Buxbaum JD. Neurobiology of Mental Illness. Oxford, UK: Oxford University Press; 2013.
Phillips RG, LeDoux JE. Differential contribution of amygdala and hippocampus to cued and contextual fear conditioning. Behav Neurosci. 1992;106:274-285. Abstract
Schlesser MA, Winokur G, Sherman BM. Hypothalamic-pituitary-adrenal axis activity in depressive illness: its relationship to classification. Arch Gen Psychiatry. 1980;37:737-743. Abstract
Ohmura Y, Yoshioka M. The roles of corticotropin releasing factor (CRF) in responses to emotional stress: is CRG release a cause or result of fear/anxiety? CNS Neurol Disord Drug Targets. 2009;8:459-469.
Liao W, Chen H, Feng Y, et al. Selective aberrant functional connectivity of resting state networks in social anxiety disorder. Neuroimage. 2010;52:1549-1558. Abstract
Paulesu E, Sambugaro E, Torti T, et al. Neural correlates of worry in generalized anxiety disorder and in normal controls: a functional MRI study. Psychol Med. 2010;40:117-124. Abstract
Liao W, Qiu C, Gentili C, et al. Altered effective connectivity network of the amygdala in social anxiety disorder: a resting-state FMRI study. PLoS One. 2010;5:e15238.
Kim MJ, Gee DG, Loucks RA, Davis FC, Whalen PJ. Anxiety dissociates dorsal and ventral medial prefrontal cortex functional connectivity with the amygdala at rest. Cereb Cortex. 2011;21:1667-1673. Abstract
Kim MJ, Loucks RA, Palmer AL, et al. The structural and functional connectivity of the amygdala: from normal emotion to pathological anxiety. Behav Brain Res. 2011;223:403-410. Abstract
Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386-389. Abstract
Martin EI, Ressler KJ, Binder E, Nemeroff CB. The neurobiology of anxiety disorders: brain imaging, genetics, and psychoneuroendocrinology. Psychiatr Clin North Am. 2009;32:549-575. Abstract
Norrholm SD, Ressler KJ. Genetics of anxiety and trauma-related disorders. Neuroscience. 2009;164:272-287. Abstract
Hariri AR, Holmes A. Genetics of emotional regulation: the role of the serotonin transporter in neural function. Trends Cogn Sci. 2006;10:182-191. Abstract
Heim C, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry. 2001;49:1023-1039. Abstract
Vergne DE, Nemeroff CB. The interaction of serotonin transporter gene polymorphisms and early adverse life events on vulnerability for major depression. Curr Psychiatry Rep. 2006;8:452-457. Abstract
Ouellet-Morin I, Odgers CL, Danese A, et al. Blunted cortisol responses to stress signal social and behavioral problems among maltreated/bullied 12-year-old children. Biol Psychiatry. 2011;70:1016-1023. Abstract
Wu CT, Morris JR. Genes, genetics, and epigenetics: a correspondence. Science. 2001;293:1103-1105. Abstract
Perroud N, Paoloni-Giacobino A, Prada P, et al. Increased methylation of glucocorticoid receptor gene (NR3C1) in adults with a history of childhood maltreatment: a link with the severity and type of trauma. Transl Psychiatry. 2011;1:e59.
Kinnally EL, Capitanio JP, Leibel R, et al. Epigenetic regulation of serotonin transporter expression and behavior in infant rhesus macaques. Genes Brain Behav. 2010;9:575-582. Abstract
Perroud N, Salzmann A, Prada P, et al. Response to psychotherapy in borderline personality disorder and methylation status of the BDNF gene. Transl Psychiatry. 2013;3:e207.
Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. 2006;9:519-525. Abstract

